In Part 1, I outlined how and why paradigm shifts change. When what we see challenges long held beliefs, we are forced to alter the way we view things. I also stated that I believe the way we have classically treated the vast majority of musculoskeletal pain is drastically in need of a paradigm shift, and briefly introduced the current model. In Part 2 I will outline the shortcomings of this model (termed Pathoanatomical diagnosis and treatment), and discuss where it has led us.
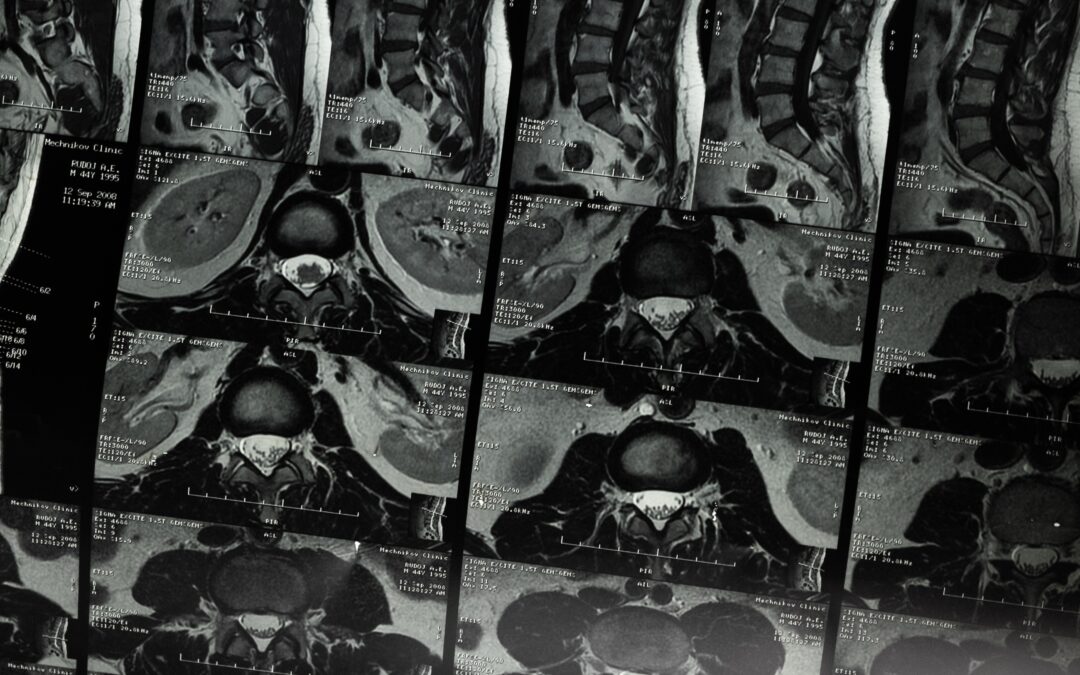
Pathoanatomical diagnoses are often determined through patterns from a patient’s history, findings from orthopedic tests and palpation, and results from imaging (e.g. x-ray or MRI). The problem with this approach is that even though these methods of investigation were designed to determine the exact tissue causing pain (e.g. spinal disc, hip labrum, shoulder rotator cuff, etc.), they are not very accurate in many cases. Histories can be misleading, orthopedic tests and palpation are often unreliable, and the prevalence of false positives and negatives on x-ray and MRI are very high for many musculoskeletal pathologies.
For instance, many people without pain have a disc herniation or rotator cuff tear show up on an MRI. There is plenty of research to validate it. Since this is the case, if a rotator cuff tear or disc herniation is discovered on an MRI of someone with pain, how would we know if it was actually the cause of symptoms? How would we know if it was relevant? These questions become even more important without an overt causal mechanism or robust clinical exam findings to support the relevance of the imaging finding. Every clinician reading an X-ray or MRI should have these questions running through their mind. Unfortunately most don’t, and end up making decisions regarding patient care on a faulty paradigm.
In addition, if we actually do happen to determine the tissue causing pain, that information alone doesn’t tell us how to treat it. A pathoanatomical diagnosis, accurate or not, oftentimes doesn’t tell the clinician how to correct the problem. Out of this confusion, many different treatments for the same pathoanatomical diagnosis have emerged over the years. Many medical disciplines, whether it be a chiropractor, orthopedist, physical therapist, interventionalist, massage therapist, surgeon etc. (not to mention different disciplines within each discipline), have unique approaches to the same pathoanatomical diagnosis. Some of these treatments are backed by research for a given condition while others are dogmatic, and obviously not every approach can be right.
Additionally, even if a treatment has been proven to be effective for a given condition, as we saw earlier there are still problems with accurately diagnosing that condition. Failed treatments, poor outcomes, and confusion often result. When this happens, patients are often quickly escalated to costly and aggressive treatments that they would have no business receiving if they were properly diagnosed and treated.
For these reasons, the scientific literature has been telling us for years to get smarter about pain.
Why we need a paradigm shift
The big problem is that this is not a small issue. We’re not talking about a few mismanaged cases here and there. About 2% of the United States Gross Domestic Product (GDP) is paid out in musculoskeletal costs each year, totaling hundreds of billions of dollars. Invasive treatments are on the rise. Over 1.5 million spinal surgeries are performed each year in the United States. Nearly 800,000 knee replacement surgeries are performed each year. About 500,000 shoulder surgeries are performed each year. The number of steroid injections performed are rapidly rising year after year. Even though in a substantial number cases of these procedures aren’t warranted, it should be noted that in many the still are. Even with all these expensive and invasive treatments, however, the rate of chronic pain is still increasing. Roughly 1 out of 3.5 people in the United States is living with chronic pain. In addition, we have created the biggest drug epidemic in our nation’s history, the opioid crisis, in large part because of our failure to adequately treat pain. With the pathoanatomical model as our guide, pain is America’s number one health problem.
The way we make decisions regarding musculoskeletal pain is drastically in need of a paradigm shift. The billion dollar question, however, is what is there to shift to? In Part 3 I will introduce the answer to that question, the McKenzie Method.